Stellefson M, Wang M, Balanay JG, Wu R and Paige S (2020). Latent Health Risk Classes Associated with Poor Physical and Mental Outcomes in Workers with COPD from Central Appalachian U.S. States. International Journal of Environmental Research and Public Health 17(18): 6798. doi:10.3390/ijerph17186798
This article belongs to the IJERPH Special Issue, Health-Related Quality of Life and Chronic Diseases: A Call to Action.
Abstract
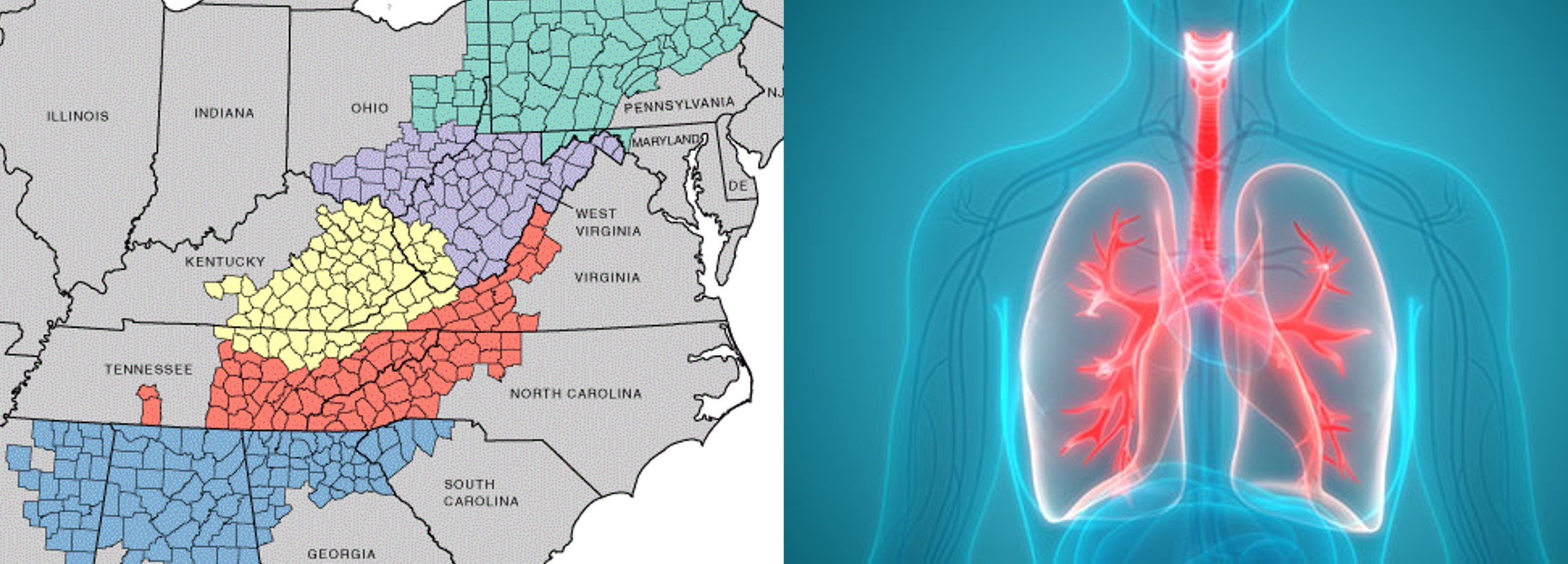
Adults who work in the Central Appalachian region of the United States (U.S.) are disproportionately affected by Chronic Obstructive Pulmonary Disease (COPD). While there is a socio-demographic profile of adults with COPD who are at increased risk for physical and mental distress, the risk factors that uniquely affect the health-related quality of life (HRQoL) of Central Appalachian workers with COPD are unknown. Therefore, we conducted a latent class analysis of 2016 and 2017 Behavioral Risk Factor Surveillance System data from 1326 currently employed adults with COPD living in four U.S. states (KY, NC, TN, and WV) within the Central Appalachian Region. Drawing from the social ecological model, we identified associations between theoretically informed risk indicators—comorbid health conditions, substance use and abuse, and limited access to healthcare—on three HRQoL variables, including infrequent (0–13 days) or frequent (≥14 days) physical distress, mental distress, and limited activity due to poor health over the past 30 days. Workers at high risk for comorbid conditions reported more frequent physical distress, mental distress, and activity limitations as compared to those at low risk. Workers reporting difficulty accessing healthcare were no more likely to report physical or mental distress when compared to workers with adequate access to healthcare; however, those with limited healthcare access did report more frequent activity limitation due to poor health. Interestingly, workers with COPD at high risk for substance use and abuse were no more likely to report poor HRQoL outcomes compared to those at low risk. Our findings have important implications for addressing indicators of poor health among Central Appalachian workers with COPD, especially those living with multiple comorbidities.